Seborrhea

Seborrhea on the scalp and seborrhea on the face are terms that are often labeled as seborrheic dermatitis, but in fact, seborrhea is a technical term for the excessive secretion of sebum from the sebaceous glands.
An article from the National Library of Medicine highlights the link between the production of sebum-fat on the scalp and the appearance of dandruff and seborrheic dermatitis on the skin and scalp. It occurs in more than 50% of the adult population. But it should be emphasized that the term seborrhea means increased secretion of sebum, not seborrheic dermatitis. →
On the other hand, the Cleveland Clinic article claims, that about 11% of the population in the US has problems with seborrheic dermatitis. Also, the Croatian website Pliva Zdravlje reports that seborrheic dermatitis occurs in about 2-5% of the total population in our region. From this, we can conclude that there are several theories regarding this, but experiences with seborrhea and seborrheic dermatitis show that the problem is very widespread.→→
Dry follicular seborrhea is a condition of dry, thin hair as a result of crystallized oil in the follicle. It is an anomaly that can appear on the head or face, but we will talk about that in another text.
Oily seborrhea, on the other hand, is a condition in which the oil (sebum) is liquid and flows over the scalp and hair. Hair is greasy, and heavy, with an unpleasant smell. The skin on the head and scalp are oily, and the oil spills from the roots to the tips. This is typical oily hair.
If you have dandruff flakes on your scalp accompanied by itching, redness, and inflammation, then you are in the right place. Your problem is not seborrhea, but seborrheic dermatitis, seborrheic dermatitis with a psychosomatic component, or psychosomatic dermatitis.
The main difference between dandruff and seborrhea is that dandruff has a distinctive appearance. It is small, white in color, and most oily. It is very often accompanied by itching, while redness with the appearance of white or yellow scales appears in places affected by seborrhea.
The difference between seborrhea, seborrheic dermatitis, and dandruff
Seborrhea is increased oil secretion by the sebaceous gland, there is only oiliness involved, and it does not cause itching.
Dandruff, which can be dry or seborrheic, that is, flaky skin mixed with oil, also does not cause itching. When it comes to dandruff, the flakes are characteristically white, there is no redness, no irritation, and no itching.
Seborrheic dermatitis is a chronic type of skin inflammation, the scales are of characteristic yellowish color, larger than dandruff, and are strongly stuck to the scalp. In addition, the area is red, the skin is irritated and itchy. Seborrheic dermatitis is a chronic inflammation of the skin that occurs on the parts where the sebaceous glands are the most numerous and dense.
Seborrheic dermatitis
Seborrheic dermatitis: itching and dandruff accompanied by erythema, the appearance of redness in the central part of the head, which can spread from the scalp up to 1 cm to the skin of the forehead.
On the Internet, you will come across the term seborrhea on the scalp as a synonym for seborrheic dermatitis very often. But if we use the correct professional terminology, seborrheic dermatitis is the correct term for this condition, while seborrhea on the scalp means increased secretion of sebum on the head, as we already wrote in the introduction.
But seborrhea, as increased secretion of sebum through the sebaceous glands, whether dry or oily, is the main cause of dandruff and seborrheic dermatitis, which is why it is often associated with this in professional articles.
In seborrheic dermatitis, itching and erythema on the scalp are caused by the oxidation of fatty acids, but only when the percentage of the fungus pityrosporum ovale (Malassezia in D/SD) reaches a sufficiently large proportion of the bacterial flora (83%).
Bacterial flora is the natural protection of the scalp, consisting of sweat, tallow (sebum), dead cells, physiological bacteria and fungi (among them pityrosporum ovale – Malassezia in D/SD), and other oils produced by the skin. When in balance, it has a self-sterilizing and germicidal effect.
When we have dry dandruff, the percentage of pityrosporum ovale fungus on the scalp exceeds the normal percentage of bacterial flora of 40%. In oily dandruff, this percentage exceeds 73%. Neither dry nor oily dandruff causes itching. Itching and erythema are signs of seborrheic dermatitis.
When pityrosporum ovale reaches 83% of the bacterial flora, it releases fatty acids from the sebum. They oxidize and become very irritating to the scalp, causing erythema and itching.
In seborrheic dermatitis, the erythema is concentrated only in the central part of the scalp. In the most severe cases, erythema, redness, and itching spread beyond the scalp to the skin of the forehead.
Seborrhea on the face

Seborrhea on the face is the correct professional meaning for increased secretion of sebum and occurs mainly on the parts of the face where there are the most sebaceous glands, namely on the forehead, nose, and chin. In these parts, the concentration of sebaceous glands is the highest, that is, the glands themselves are larger, so a larger amount of sebum is secreted.
Facial seborrhea is a term people often use for facial seborrheic dermatitis or seborrheic dermatitis with a psychosomatic component. In this chapter, we’ll focus on that topic, because that’s probably how you’ve been doing your search.
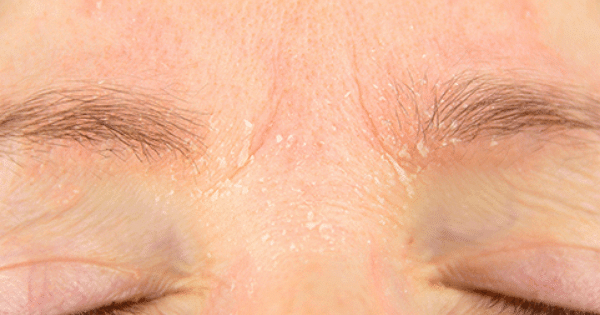
But seborrhea on the face (properly speaking, seborrheic dermatitis on the face) can also be present on the temples, on the eyebrows and eyelashes, on the sternum, between the shoulder blades, and on other parts of the body when it comes to seborrheic dermatitis with a psychosomatic component.
The pictures of seborrhea on the face or seborrheic dermatitis on the face in this gallery can confirm if you are in the right place, but keep in mind that the problem can occur in all of these places, or only in some.
Seborrhea on the face or seborrheic dermatitis on the face can be of different intensities, depending on the person, so the condition does not have to be as pronounced as in these pictures.


Seborrheic dermatitis – face cream

Seborrheic dermatitis is a relapsing chronic inflammatory disease, which most often affects seborrheic parts of the skin with increased activity of sebaceous glands. This disease is characterized by an inflammatory reaction, which includes redness and peeling of the skin in the affected areas. It occurs more often in men than in women, especially at an earlier age.
Seborrheic dermatitis is an anomaly on the scalp characterized by peeling of the epidermis, redness, inflammation, and itching, especially in the central part of the scalp. When it appears on the face and other parts of the body, it mostly occurs on the parts where the activity of the sebaceous glands is the greatest, that is, on the parts where the secretion of sebum or seborrhea is the greatest.
As a rule, the problem occurs more often in men, because men have oilier skin than women due to the effect of androgens, male sex hormones. Androgens (male sex hormones) stimulate the work of the sebaceous glands, while estrogens (female sex hormones) inhibit their work. This is why women generally have less oily skin and scalp than men.
Seborrheic dermatitis is not contagious and is not transmitted by hairdressing combs.
Seborrheic dermatitis is a long-term condition. It may take a whole series of repeated treatments before the symptoms disappear. The downside of seborrheic dermatitis is recurrence regardless of treatment.
Seborrheic dermatitis is recurrent, that is, it occurs several times in a lifetime, even if we have brought it under control with successful treatments. Like herpes, it remains present in cases of severe stress, reduced immunity, or psychophysical exhaustion, and it appears again, sometimes in a more severe form.
Often the condition worsens during treatment, especially in the spring, during the same periods as the stomach ulcer. Experience shows that people who suffer from stomach ulcers also often suffer from seborrheic dermatitis.
Seborrhea on the face or seborrheic dermatitis on the face is treated with different face creams. There are many creams on the market intended for seborrhea on the face or seborrheic dermatitis, and customers’ experiences with them differ.
If we want to effectively treat a problem, we must always start from the cause. The cause of seborrhea or seborrheic dermatitis on the face is fungi on the skin. The fungus pityrosporum ovale (Malassezia in D/SD) is present on the skin and scalp and feeds on sebum, namely fats. Like all fungi, it thrives in a moist, warm environment with sufficient food for its reproduction.
Face creams for seborrhea or seborrheic dermatitis must have an antimycotic (antifungal) effect. Second, they must remove the excess sebum that feeds the fungi but also act on the result, namely redness, inflammation, and itching.
1% cortisol cream is rubbed into the areas behind the ear, between the nose and lips, the edges of the eyelids, and the root of the nose, 2 to 3 times a day. When the situation is under control, then the cream application is reduced to once a day.
The active ingredients in antimycotic face creams and lotions are tea tree (melaleuca alternifolia), cajeput (melaleuca leucadendron), olamine acid derivatives, and various corticosteroids or cortisol creams.
Corticosteroids and cortisol creams and facial lotions for seborrhea on the face or seborrheic dermatitis on the face are very effective, but they cannot be used continuously, and if we overuse them, they become ineffective over time because they destroy the natural protection of the skin (bacterial flora).
In natural face creams and lotions for seborrhea on the face or seborrheic dermatitis on the face, tea tree (melaleuca alternifolia) is often used, which, in addition to having an antimycotic effect, also has a dermopurifying effect, that is, it removes excess fat from the skin. But this is not always enough, because it is necessary to act on sebum production with sebo-normalizing active ingredients, such as sausage tree (Kigelia Africana). In this way, the secretion of sebum is decreased, and thus the amount of food for the fungus pityrosporum ovale (Malassezia in D/SD) is reduced.
There are various ingredients in face lotions and creams for seborrhea on the face or seborrheic dermatitis on the face that have a soothing, anti-redness, anti-itching, and anti-inflammatory effect.
Less natural ingredients in face creams for seborrheic dermatitis are, for example, corticosteroids, which include, for example, ketoconazole, miconazole, and metronidazole. It is necessary to keep in mind that they are synthetic copies of cortisol (adrenal gland hormone), which has an anti-inflammatory effect, and as such, they should not be misused. They should not be used more than the amount according to the instructions, and long-term use often causes the skin to get used to it, thus reducing or losing its effectiveness.
Partially natural ingredients such as olamine acid derivatives (piroctone olamine) and natural ingredients such as witch hazel, sweet almond oil, oats, marine collagen, hops, etc. can be a good alternative because they can be used continuously and are often sufficient, especially when it comes to milder forms of the anomaly.
Experience shows that marine collagen is one of the best active ingredients in creams and lotions for seborrhea on the face or seborrheic dermatitis on the face because it contains a large amount of omega-3 fatty acids that act as an anti-inflammatory, anti-itching, anti-redness, and soothing.
Likewise, experiences with creams and lotions for seborrhea on the face or seborrheic dermatitis on the face show that often the cream is not the best solution, because it is too oily.
Since seborrhea or seborrheic dermatitis with a psychosomatic component is characterized by a large amount of fat, therefore an emulsion in cream is not the best solution. Drops or serums have proven to be more suitable for treating problems on the face, especially when they are concentrated in drops with a high concentration of active ingredients.
Seborrhea on the head
Seborrhea on the scalp: flakes, itching, inflammation, and redness on the central part of the scalp or seborrheic dermatitis.
The pictures show that the problem is present in the central part of the head, where the largest concentration of sebaceous glands is.


The causative agent is the fungus pityrosporum ovalis or Malassezia, which feeds on sebum (fat) and can reach 83% of the bacterial flora on the scalp. (https://en.wikipedia.org/wiki/Malassezia)
Many people confuse dandruff and seborrhea. In both cases, these are skin phenomena that most often occur on the scalp. They represent an aesthetic problem, but they can also be very unpleasant due to all the symptoms that accompany them. The main difference between dandruff and seborrhea is that dandruff has a distinctive appearance. It is small, white in color, and mostly oily. It is very often accompanied by itching, while redness with the appearance of white or yellow scales appears in places affected by seborrhea.
As we have already written in the above chapters, people often confuse dandruff and seborrhea on the head or seborrheic dermatitis.
Dandruff is characterized by flakes with or without oil, but completely without inflammation, redness, and itching. On the other hand, seborrhea of the scalp or seborrheic dermatitis is characterized by redness, inflammation, and itching, especially in the central part of the head with yellowish scales that are strongly stuck to the scalp.
Scabs on the head
Scabs on the head, in addition to an aesthetic problem, can cause severe itching that irritates a person and spoils his mood. Itching can often be very unpleasant, and with each subsequent scratching the itching intensifies, that is, the scabs increase in size and become a bigger problem.
Scabs and scabs on the scalp are mostly the results of scratching due to an itchy scalp. We have described the causes of the problem in detail above, but scratching and thus the formation of scabs on the head is a problem that deserves special attention.
Scabs on the head occur as a result of scratching with nails, because this creates scratches and wounds that can become additionally infected, the fungi penetrate deeper into the scalp, and thus the problem of seborrhea or seborrheic dermatitis is further intensified.
If our scalp itches, it is necessary to use an anti-inflammatory, soothing preparation as soon as possible to reduce the need for scratching. It is ideal to choose a preparation that we can always have with us and simply apply it to the itchy part instead of scratching.
Scabies on the head can also be avoided by scratching with the tip of the fingers or knuckles and never with nails.
Psoriasis is a very widespread pathological cause that most often develops on several parts of the body, in this case, white crusts appear that look dry. Most of the time it is indistinguishable from dandruff, the main symptom is itching, you can use emollient products for dandruff and dry skin to relieve and control the disorder.
Scabs on the head can also be a consequence of psoriasis, which, unfortunately, is an incurable skin disease that, in addition to the scalp, also occurs on the elbows, knees, and other joints. Psoriasis is characterized by a white crust on the affected parts, the skin is extremely dry, and when cracked, it can bleed and form scabs on the head and body.
As we said, this is an incurable disease, but preparations based on cajeput and marine collagen have proven successful in alleviating the problem.
Fungi on the skin
A large number of different forms and types of fungi can cause health problems when they break through our body’s defenses. In addition to systemic fungal infections (mycosis) that affect the entire organism, yeast infections and mold infections, which we call fungal infections of the skin or dermatomycoses (commonly known as “fungi on the skin”), are much more common.
Fungi on the skin can be caused by various fungi (mycosis), yeasts, and molds, and we can get infected with them in public places such as gyms, swimming pool changing rooms, and the like.
Fungi on the skin and a disruption of the bacterial flora, namely the development of the physiological fungus pityrosporum ovalis or Malassezia, are not the same. Natural preparations for skin fungus are often based on tea tree or cajeput, but we recommend that the problem be solved with targeted preparations after consultation with a doctor, pharmacist, or dermatologist. →
Fungi on the hands
If there are fungi on the hands, it is surely a contagious fungal infection, and it is often confused with other skin diseases that appear on the hands. Dermatophytes are the most common cause of fungal infections on the hands. Dermatophytes are defined as a type of fungus. Almost every person has a certain percentage of probability that they will have fungi on their hands once in their life, more precisely every person will develop a fungal infection on their hands.
Fungi on the hands are the result of a fungal infection that can often be confused with other changes on the hands. Dermatophytes are a type of fungi that can cause fungal infection on the hands.
Fungi on the hands of dermatophytes are contagious, namely, we can get them if we are in contact with another body that has a fungal infection. It can be another person, animal, soil, or other surfaces on which the fungi have settled. They usually appear on the feet or groin, but hand fungi as a result of a dermatophyte fungal infection are also very common.
Another common cause of hand fungi and this type of infection is scratching or touching another part of the body where there is a fungal infection. Most often, fungal infections occur on the feet, but also in the crotch. However, if the cause of the fungal infection is determined to be a dermatophyte infection on the hands, or rather the spread of a dermatophytes fungal infection, then you could have gotten it from another person who has it, from the soil or the earth you touched, or from an animal you touched, if the animal has a fungal infection.
Hand fungus presents with an irritating, itchy rash that can affect one or both hands of a person who has a fungal infection. Fungal infection usually starts on the palms and can spread to the rest of the hands and the fingers of both hands. If you have fungi on your hands, there may be redness in the form of a circle on a certain part of the skin, and in the middle of that circle, the skin looks like it has healed.
Fungus on the hands is characterized by itching, which is not a consequence of seborrheic dermatitis, but a fungal infection. It usually starts on the palms and then starts to spread to other parts of the hand.
Redness often appears in the form of a circle with a central part that looks like a healed wound, and blisters between the fingers filled with a clear liquid. After the blisters burst, calluses and skin discoloration appear, which is especially visible in people with darker skin.
With hand fungi, the skin is scaly, dry, and intensely itchy, which is why people often think it’s dermatitis. But as with dermatitis, the cause is a fungus that thrives in a moist, warm place, and in this case, it is also contagious.
It is necessary to reduce moisture on the hands and other affected parts. It is necessary to dry the affected parts well, if they are on the feet, regularly change socks, and use specific antimycotic preparations. There are also oral medications available that can act on the problem internally rather than just topically but check with your doctor or pharmacist about how to use them.
This symptom occurs if you got a fungal infection from an animal or from the soil you touched with your hands. Dry, scaly skin may also appear, it may be itchy, and this itching may spread to a larger area on the hands.
Also, small blisters may appear on the fingers or palms that are filled with fluid. In addition, skin discoloration can occur if you have had a fungal infection for a long time, and if it does not go away, it causes severe and irritating itching. These symptoms most often appear after the infection has been transmitted from person to person.
