Dermatitis
Seborrheic dermatitis
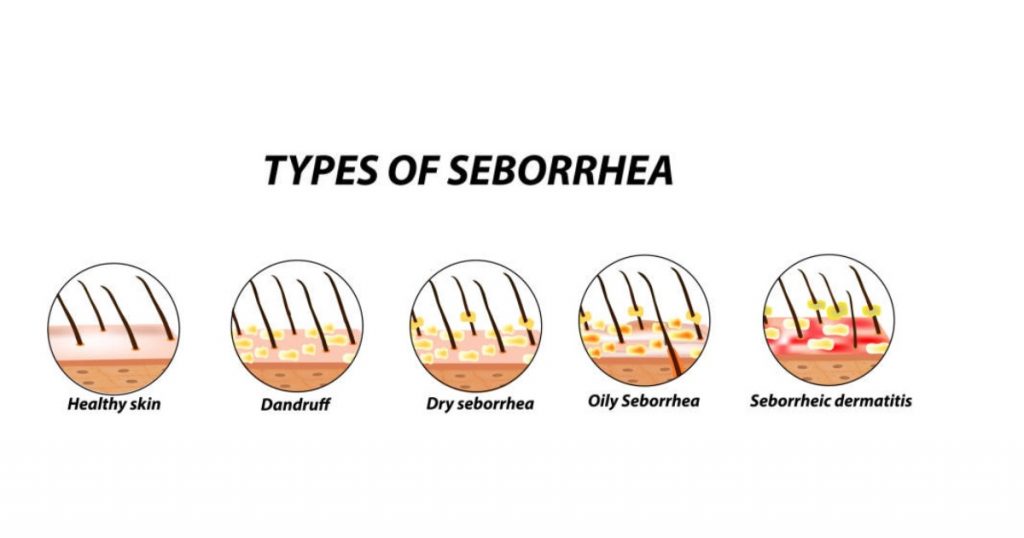
Seborrhea on the head and seborrhea on the face are terms that are very often used to define seborrheic dermatitis, but essentially, seborrhea is a technical term for the excessive secretion of sebum by the sebaceous glands.
If you have flakes of dandruff, itching, redness, inflammation, and sores on your scalp, then your problem is not seborrhea, but seborrheic dermatitis, seborrheic dermatitis with a psychosomatic component, or psychosomatic dermatitis.

How to distinguish between dandruff, seborrhea, and seborrheic dermatitis?
Seborrhea is an increased secretion of fat from the sebaceous glands, and it is only about dry or oily fat that does not cause itching. Hair and scalp are greasy and cause, for the most part, an aesthetic problem.
Dandruff is recognizable by its small scales, white in color, without itching, redness, and erythema.
Seborrheic dermatitis is a chronic inflammation of the skin, the scales are larger than dandruff, yellowish in color, and can be stuck to the scalp in multiple layers. The area is red, sores are often present, and an irritating itch is present.
Bacterial flora, natural skin protection consists of sebum (fat), sweat, dead epidermal cells, physiological bacteria and fungi (among others Pityrosporum ovale – Malassezia in D/SD), and other fats produced by the skin. When in balance, it has a germicidal and self-sterilizing effect.
In dry dandruff, the percentage of the fungus Pityrosporum ovale exceeds the normal presence in the bacterial flora by up to 40%. With oily dandruff, the presence is over 73%, but even then there is still no itching or erythema. When Pityrosporum ovale reaches 83% presence in the bacterial flora, it begins to secrete fatty acids from sebum, which in oxidation processes cause inflammation, itching, redness, sores, and scabs.
What is seborrheic dermatitis?
Seborrheic dermatitis is a papulosquamous disorder that occurs on skin rich in sebaceous glands and sebum. It appears in the form of seals, which itch, and is accompanied by peeling of the skin. In case sores are created by scratching, burning and redness occur. Dandruff is yellowish in color, very often greasy and moist. It most often occurs on the capillitium, but it can also occur on the face, chest, back, and other parts of the body that have a lot of sebaceous glands.
Seborrheic dermatitis is not contagious and cannot be passed from one person to another. It cannot affect general health, but it causes an aesthetic problem that can be bothersome. Over time, it can lead to significant hair loss, because although it is a skin problem, it has a lot of impact on the health of the hair and its appearance. Dandruff deposits on the scalp create a barrier and prevent normal hair growth, leading to thinning and hair loss.
Seborrheic dermatitis is caused, in addition to sebum, by the fungus Pityrosporum ovale, which is part of the bacterial flora, as well as various immune abnormalities. Seborrheic dermatitis is a long-term skin condition and is recurrent, ie. it appears many times in life, even if we have brought it under control with successful treatments. Like herpes, it remains present, so in cases of a strong drop in immunity, stress, or psychophysical exhaustion, it knows how to return even in a more severe form.
Clinical picture
Seborrheic dermatitis is not the same as regular dandruff, so if you struggle with this problem, it can be very frustrating. Your shoulders are constantly full of white or yellowish scales, which are not at all small and unnoticeable, and your hair gets greasy very quickly and always looks messy. The scalp is covered with a layer of dandruff, and when you scratch, dandruff spreads through the hair. Over time, hair begins to fall out and hair loss occurs.
Dandruff, redness, erythema, and itching do not stop only on the hair but spread over the face, forehead, nose, and eyebrows. They can also appear in the ear, on the chest, on the shoulder blades, and so on. The condition worsens with increased air humidity when the seasons change (it is in remission in summer, worsens in autumn, and drastically worsens in winter when the air humidity is the highest. In spring, the condition is milder than in winter). It varies from mild scaling, which occurs in lesions (limited areas), to the appearance of severe squamous deposits, which can cover the entire scalp.
Symptoms of seborrheic dermatitis
Symptoms of seborrheic dermatitis manifest as:
• Large scales of dandruff
• Itchy scalp
• Scratching can lead to secondary bacterial infections, wetting, sores, and scabs
• Red and inflamed seals on the scalp, sores, and scabs
• Unpleasant smell of hair and scalp
• Dandruff deposits in the form of cradle caps in adults

Symptoms of seborrheic dermatitis can also appear on other parts of the body:
• Face, eyebrows, around the edges of the eyelids (the result can be inflammation of the eyelids – blepharitis), around the nose area, nasolabial folds, behind the ears, and in the external ear canal
• Chest, back, underarms, navel area, thighs, and in places where there are bends and folds on the body
In whom does seborrheic dermatitis occur?
Seborrheic dermatitis occurs in both sexes, but a more severe clinical picture is more common in men, with more prominent symptoms. It most often occurs in the third and fourth decade of life, and also in the period of adolescence, due to sudden and intensified hormonal changes. It can also occur in babies, usually around ten weeks after birth, and it is a cradle cap, which is temporary and usually disappears by the age of three.
It is estimated that around 10-20% of the world’s population has seborrheic dermatitis problems. The main characteristic of seborrheic dermatitis is its persistence, because it very often returns, just when we thought we got rid of it.
Seborrheic dermatitis – causes
The most common causes of seborrheic dermatitis are:
• The contribution of the Pityrosporum ovale fungus is high, due to its additional effect on enhancing lipid activity (it releases more fatty acids – the main factor of inflammation) and its ability to activate inflammatory processes.
• Itching, redness, inflammation, wounds, and scabs, are caused by the oxidation of fatty acids, but only when the percentage of the Pityrosporum ovale fungus exceeds 83% as part of the bacterial flora.
• Seborrheic dermatitis is most often hereditary, due to disturbances in the function of the sebaceous glands, and increased secretion of fat, which results in the shortened process of scalp cell renewal. The consequence is accelerated exfoliation of keratinized skin cells.
Other possible causes of seborrheic dermatitis are:
• Hormonal changes (especially sex hormones)
• Emotional stress
• Psychiatric and neurological conditions (depression and Parkinson’s disease)
• Weakened immune system
• Endocrine gland diseases
• Diet (fast food, fatty and spicy food, alcohol…)
• Use of certain medications
• Use of aggressive and inappropriate cosmetic products (shampoo, conditioner…)
• A change in the pH value of the skin
• Aggressive skin irritations (chemically or by exposure to a large number of microorganisms)
• Damage caused by aggressive scratching or scraping
• Climatic conditions (extremely high or low temperatures, increased air humidity, wind…)
Seborrheic dermatitis occurs in episodes because it is a chronic skin problem, so periods of improvement and worsening of symptoms alternate.
Aggravation of seborrheic dermatitis occurs due to:
• Fatigue, mental and physical exhaustion
• Stress
• Use of inappropriate shampoos, shower gels, soaps…
• The seasons very often determine the rhythm of the inflammatory process, so it generally worsens during the winter period.

The solution
With proper care and appropriate treatments, seborrheic dermatitis can be kept under control, without major escalations and consequences, such as hair loss. If we thoroughly approach the solution, we must start from the cause, and the main cause of seborrheic dermatitis is the increased presence of the fungus Pityrosporum ovale (Malassezia in D/SD) on the skin. Like all fungi, a moist and warm environment suits it perfectly, and since it feeds on fat, the excess sebum provides it with additional food.
Therefore, if we want to stop its reproduction and the damage it does, we should, to begin with, deprive it of what is most beneficial to it, namely moisture and food – fat.
Treatments, creams, and lotions used for seborrheic dermatitis must, first of all, have antimycotic (antifungal), degreasing, anesthetic (anti-itching), and inflammatory (anti-inflammatory) effects.
Corticosteroids and cortisol creams are very effective but are used for a very short period, so if you break through that time limit and overuse it, you can do much more harm than good to the skin.
The natural active ingredients in preparations for solving seborrheic dermatitis have no contraindications and no limited time of use, and at the same time, they have a very high level of effectiveness.
The natural active ingredients that have been proven to have the most beneficial effects are:
• Marine collagen: contains a large amount of omega 3 fatty acids that have an anti-inflammatory, anti-itching, anti-redness, and soothing effect
• Tea tree (Melaleuca alternifoglia): besides being antimycotic, it also has a dermopurifying effect (removes fat from the skin)
• Kigelia Africana: sebonormalizes and acts directly on the sebaceous glands, regulating excessive sebum secretion, which automatically reduces the amount of food for the Pityrosporum ovale fungus.
• Cajeput: a tropical plant with strong antimycotic performance
• Witch hazel, sweet almond oil, oat extract, hops, and so on: they can be used continuously in the composition of skin wash, without any consequences, for a long period of time.
Contact dermatitis
Contact dermatitis is a red, itchy rash. It occurs as a result of skin contact with an irritating agent – it causes irritation and allergy. Contact dermatitis is an acute inflammation of the skin, caused by irritants or allergens. The first symptom is itching and rash on the skin, which ranges from erythema to the formation of blisters and rhagades.
It most often occurs on the hands or near them, but also on other uncovered parts of the body. The rash is not contagious and not life-threatening, but it can be very unpleasant and impair the quality of life. In order to approach the treatment of contact dermatitis, it is crucial to find the substances to which the sensitivity occurs and to avoid them.

How does contact dermatitis occur?
Contact dermatitis occurs as an allergic reaction caused by the irritating action of a substance. The most common irritants are soaps, detergents, dust, antiseptics, solutions, machine oil, cement, soil, water with a high concentration of chlorine (in swimming pools), certain types of cosmetics, and some plants.
Types of contact dermatitis
• irritant contact dermatitis (ICD), which accounts for 80% of all causes of contact dermatitis, is a non-specific inflammatory reaction to substances with which the skin comes into contact, without activation of the immune system. First of all, various chemicals are included (acids, bleaches, salts, solutions, metals…), detergents (abrasives, gels, soaps…), shampoos, airborne substances (sawdust, wool dust…), plants (pepperoni, some types of flowers…), artificial fertilizers, pesticides.
• phototoxic dermatitis occurs as a local change on application spots (perfume, coal tar…) or ingestion (example: drug Psoralen) of certain substances, which create harmful free radicals only after absorption of ultraviolet rays.
• allergic contact dermatitis (ACD) is a reaction of cellular hypersensitivity and occurs when an agent to which a person is sensitive triggers an immune reaction on the skin. An allergic reaction affects only the area that was in contact with the allergen. The reaction can be triggered by something else that can enter the body through drugs, food, or medical and dental procedures. It has two phases: antigen sensitization and reexposure response.
Substances that cause allergic contact dermatitis are:
- Medicines (antibiotic creams and oral antihistamines)
- Formaldehyde (preservatives, disinfectants, clothes…)
- Nickel (found in metal buckets, jewelry…)
- Personal hygiene products (nail polish, hair dyes, lotions, deodorants…)
- Substances that can be found in cosmetics, sweeteners, perfumes, dental hygiene products…
- Plants (poison ivy, mango containing the urushiol allergen…)
- Products that cause a reaction to the sun, some sunscreens, and oral medications…
- In children, it occurs from wearing diapers, wet wipes, and dyed clothes…
People with increased risk factors are those who engage in certain occupations and hobbies. These are primarily health workers, construction workers, car mechanics, metal turners, hairdressers and beauticians, divers and swimmers (rubber masks), farmers, and people working with food. The rash appears within a few minutes to a few hours from contact and can last 2-4 weeks.

Symptoms of contact dermatitis are:
- Itching
- Red rash
- Dry, flaky, cracked skin
- Bumps and blisters
- Burning sensation and swelling
Atopic dermatitis
Atopic dermatitis is an inflammatory chronic disease accompanied by dry skin that is prone to itching and irritation. The word “atopic” itself refers to a group of hereditary diseases and is often associated with other diseases. Atopic dermatitis is the most common benign disease with a recurrent course because there are phases of remission (complete recovery of all signs and symptoms) and phases of exacerbation (return of symptoms and worsening of all clinical parameters).

About 2% of the world’s population has a problem with atopic dermatitis, which means that it has a high frequency. It is not contagious and most often affects babies from the 3rd month of life, then the symptoms slowly weaken (they can disappear completely by puberty), but it can also appear at an older age.
Atopic dermatitis and eczema are often thought to be the same, but they are not. Eczema includes a large number of different inflammatory diseases, and atopic dermatitis is only one of them, i.e. the most common type, and therefore is often used in the same context.
Symptoms of atopic dermatitis
The first and most common symptoms are:
- Dry itchy skin (pruritus)
- Scabies behind the ears and a rash on the cheeks, arms and legs
- Red and inflamed skin because the immune system is highly activated
- Thinned and fluffy skin from constant scratching (lichenification)
- Hyperpigmentation and small bumps on the skin may appear, which turn into scabs and infected sores due to scratching
- It can affect the area around the eyes, eyelids, eyebrows, and eyelashes, where scratching changes the color of the skin
- Some people may develop an extra layer of skin, an atopic fold, or a Dennie-Morgan fold
- The skin loses too much moisture from the epidermis and therefore becomes very, very dry, with a reduced defense mechanism
- Skin with atopic dermatitis, due to a reduced defense mechanism, becomes very sensitive to infections with staphylococcus, streptococcus, warts, and herpes simplex…
Prevention
There is no special type of prevention, but it is definitely recommended:
- Protect the skin from moisture, irritating substances, and synthetic clothing
- Keep a cooler, stable temperature and a stable level of humidity in the room
- Avoid scratching, scraping, and rubbing as much as possible
- Avoid exposure to dust, tobacco smoke, pollen, and animal hair
- Notice in time and avoid emotional stress
- Make the most of summer and the sea, as well as the mountains, due to the benefits of changing climate
- Showering is recommended over bathing, but if you already use a bathtub, then instead of shower gel, put just a few drops of olive oil or marine collagen to give the skin fat and elasticity
- Wear only cotton clothes, because everything else makes the skin itch
- Lubricate the skin with recommended means
Atopic dermatitis in babies
All parents care that their babies’ skin is healthy, beautiful and nurtured because there is nothing more beautiful and soft than a baby’s skin. But, babies whose skin is sensitive, bright, and transparent, are much more susceptible to various irritating skin conditions, the most common of which is atopic dermatitis.

Atopic dermatitis in babies is a chronic skin condition and is actually a type of eczema. It manifests as a scaly and red rash that causes inflammation and itching. According to Professor Biber, a world-renowned expert in the field of atopy, atopic dermatitis begins “in utero”, while the baby is still in the mother’s womb.
In the last decade, atopic dermatitis has been very common in babies, especially in industrialized countries. In about 60% of cases, atopic dermatitis occurs in the first year of a baby’s life, and most often in the period between 3-6 months of age. Babies who develop atopic dermatitis often have a family history of eczema, various types of allergies, and asthma… so the manifestation at an early age is most often caused by a combination of external factors and genetics. It often occurs in babies born in the winter and autumn months, more so in boys and the second child.
The first symptom of atopic dermatitis in babies is very dry, desiccated skin, which subsequently turns red and eventually develops a red rash. The most severe symptom of atopic dermatitis in babies is itching (pruritus). By scratching, the baby can injure the skin and lead to infection, so the advice and precaution are that babies wear cotton gloves. Baby itching can keep babies up all night. The baby is sleepless, crying, and in a bad mood…
Other common symptoms of atopic dermatitis in babies are:
- Very dry skin, often covered with scales
- Red rash and red, irritated skin
- Sores that may be open or covered with scabs
Redness and rough skin with small pimples appear in babies on non-convex parts of the face (chin, forehead, and cheeks). A rash and redness can appear on the bends of the elbows and knees, but quite rarely.
Symptoms of atopic dermatitis are not always constant. Sometimes they go away, and sometimes there is a “flare-up” of atopic dermatitis. There is no specific test that would fully confirm atopic dermatitis. Babies with allergies and atopic dermatitis often have elevated immunoglobulin E (IgE) in their blood. Their immune system reacts “too strongly” to certain allergy triggers and allergens, it produces more of this antibody, which can cause a reaction and lead to atopic dermatitis.
The advice to parents is, first of all, to minimize and eliminate any infection and complications. Also, regular hydration of the skin, as well as restoration of the skin’s protective hydrolipidic coating. Use very mild and non-irritating agents such as shampoos, baths, and soaps.
Atopic dermatitis in children
Atopic dermatitis in children is a chronic skin condition, a type of eczema. It manifests as a scaly and red rash that causes inflammation and itching. Atopic dermatitis is most often hereditary, so if one parent has atopic dermatitis, the chances of it occurring in the child are 30%. If both parents are atopic, the chances are increased to 70%, but still, there is a chance of up to 30% that it will not appear in the child. However, allergic rhinitis or bronchial asthma may occur.
Atopic dermatitis occurs more often in boys, in the second child, and in children born in the winter and autumn months. Both in babies and in children of all ages, atopic dermatitis often occurs in industrialized countries.
The changes are mostly localized on the inner sides of the big bends (knees, elbows, behind the ears…) as brown deposits of dry and rough skin, with extremely strong itching and quite expressed scratching marks. These changes can be constant, or they can alternately appear and recede, depending on the provoking factors.
There is no specific test that would fully confirm atopic dermatitis in children. Children with allergies and atopic dermatitis often have elevated immunoglobulin E (IgE) in their blood. Their immune system reacts “too strongly” to certain allergy triggers and allergens, it produces more of this antibody, which can cause a reaction and lead to atopic dermatitis.
According to Professor Biber, a world-renowned expert in the field of atopy, atopic dermatitis is a developmental progression of allergic diseases in childhood. It starts with the appearance of atopic dermatitis, followed by food allergy, then allergic asthma, and finally allergic rhinitis. Oral allergy syndrome (OAS), so-called contact urticaria – hives, can also occur. Hives are accompanied by swelling, redness, tickling, and itching of the tongue and throat, itching of the lips and palate, and swelling of the villi).
The advice to parents for a child with a problem with atopic dermatitis is, above all, to minimize and eliminate any infection and complications. Also, as advised in the case of atopic dermatitis in babies, the same applies to children. Regular hydration of the skin is necessary, as well as the restoration of the protective hydrolipidic layer of the skin. Avoiding all forms of allergens is mandatory, so use very mild and non-irritating agents such as shampoos, baths, and soaps.
Atopic dermatitis in adults
Atopic dermatitis (dermatitis atopic) in adults is a “trilogy” of asthma, allergic rhinitis, and atopic dermatitis, and they can occur simultaneously, alternately, or independently of each other.
Currently, about 2% of the world’s population has various problems that can be caused by atopic dermatitis, and there is a tendency for a constant increase in people with these problems, especially in urban areas. Atopic dermatitis is the progression of the development of allergic diseases in childhood, according to Professor Biber, a world-renowned expert in the field of atopy. It all starts with the appearance of atopic dermatitis, followed by the appearance of an allergy to certain types of food ingredients, after which allergic asthma may occur, and finally, allergic rhinitis may occur.
Oral allergy syndrome (OAS), so-called contact urticaria – hives, can also occur. Hives are accompanied by swelling, redness, tickling, and itching of the tongue and throat, itching of the lips and palate, and swelling of the villi).
There are many factors that influence the occurrence of atopic dermatitis. Atopic dermatitis is most often hereditary, so if one parent has atopic dermatitis, the chances of it occurring in the child are 30%. If both parents are atopic, the chances are increased to 70%, but still, there is a chance of up to 30% that it will not appear in the child. However, allergic rhinitis or bronchial asthma may occur.
Of the external factors of the environment, which can be triggering, the most common are:
- irritants (wool, soap, grease, solvents, detergents…)
- contact sensitizers (nickel, cobalt, chromium…)
- inhalant allergens (house dust, dust mites, pollen, mold, animal hair…)
- food allergens (soy, fish, wheat, peanuts, eggs…)
- microbes (Pityrosporum ovale, Candida albicans, Staphylococus aureus, Trichophyton…)
Climate has a big influence, especially the microclimate inside the house where we live. The influence of psychological factors, such as nervousness and stress, is also very large. The mechanism of atopic dermatitis is very complex, but the essence is a disturbed interaction of immunocompetent cells (T and B lymphocytes).
In adulthood and adolescence, changes in the skin are most common in the area around the lips, the backs of the hands, and the neck. Symptoms of atopic dermatitis in adults are:
- dry skin
- visible changes in the bends (elbows, knees, behind the ears…)
- intense itching and scratch marks
- white dermographism
- thinning or lack of the outer part of the eyebrow
- furrowing of the palms and soles
- facial pallor and dark circles under the eyes
Atopy is not only a skin disease
Atopy is not a skin disease, but an innate tendency to react violently to stimuli (allergens) from the external environment and an increased tendency to develop allergic reactions. It also applies to the digestive and respiratory tracts, as well as to the mucous membrane of the nose and eyes.
Atopy is not contagious
Regardless of how bad it may seem, atopy and allergies are not contagious. Therefore, isolation due to the appearance of the skin is not necessary, even during the most severe stages of deterioration.
The best cream for atopic dermatitis
For people who have a problem with atopic dermatitis, the first and very important step is prevention, which implies special and very careful care. In atopic dermatitis, the main characteristic is a disturbed bacterial flora, i.e. damage to the skin barrier and skin function, as the largest human organ. That is why the treatment of this problem always starts with appropriate care, which should restore and repair the damaged barrier function of the skin.

For maintaining hygiene and skin washing, we recommend SAP Vital Plus. SAP is a treatment with a liquid creamy emulsion, intended for all skin types, especially atopic, dry, reactive, and couperose skin, prone to inflammation. It is an extremely gentle formulation, based on almond oil, witch hazel and oats, which cleans the skin while preserving its hydrolipidic coating and the skin’s barrier function. Effectively removes smog, dust, excess oil, and makeup.
SAP contains emollients and other nutrients, such as sweet almond oil, Altea extract, and witch hazel extract. It also contains vitamins C and E, which have a protective effect on the epidermis and protect the skin from external influences, which is essential for atopic skin. The formula contains a special surfactant, an amino acid obtained from oat extract, which makes the product soluble (dissolves fat) and water-soluble (washes off with water).
Therapy for atopic dermatitis is very diverse, and the basis for care is various moisturizing emollients, which prevent drying of the skin, and therefore tension, tightness, and itching. Emollients should be used constantly, even when the skin looks perfectly healthy, for prevention.
If atopic dermatitis is in an acute phase, under the supervision of a doctor, in addition to emollients, preparations are included that should calm the inflammatory processes on the skin – local corticosteroids (in the form of creams or ointments).
