Ringworm
Ringworm: what is it?
When you have ringworm, you may think you have worms in your skin or a worm-related disease. No, you don’t. A ringworm infection is caused by a fungus, not worms.
It is likely that the name “ringworm” comes from the rash that many people see. Rashes often have a ring-shaped pattern on the skin and a raised, scaly border that snakes around the edge.
Ringworm can appear anywhere on your body. A ring-shaped pattern does not appear on the scalp, palms, nails, groin, or soles. When it occurs on the groin and soles, it has another name.
The treatment of ringworm is important no matter where it appears on the body. If left untreated, the rash tends to grow slowly and cover a larger area. Other parts of your body can also be infected. Itching can be intense when ringworm is present, but treatment can relieve it. Due to the contagious nature of ringworm, it can also be prevented from spreading to others. →
Ringworm symptoms and signs
A ringworm infection is caused by a fungus. There are many places on your body where you can get ringworm. In most cases, it causes ring-shaped patches on the skin. Ringworm, however, appears differently when it grows on the feet (bottoms and sides), scalp palms, nails, beard area, or groin.
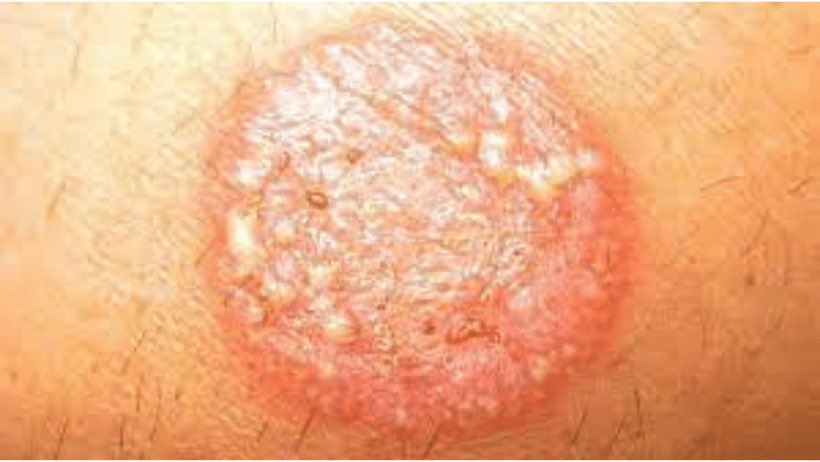
Skin with ringworm infection (Tinea corporis)
Like other forms of tinea, tinea corporis is a fungal infection of the body. Dermatophytosis (or ringworm) occurs on the arms and legs, especially if the skin is glabrous. This condition, however, can be found anywhere on the skin that is superficial.

A fungus known as dermatophyte causes tinea corporis. The disease can also be transmitted from person to person through direct skin contact with an infected individual. In addition, animal-to-human transmission is common. By touching contaminated athletic gear, personal care products, combs, bed linen, or hair brushes, the fungus can also be spread. →
The most common symptoms of a fungal skin infection are:
- Patches can be extremely itchy
- In some cases, patches can grow slowly, increasing in size and spreading to more sites
- Round-shaped, flat patches with a raised, scaly border
- Patches on colored skin are usually brown or gray
- Light-colored skin tends to have reddish or pink patches
- It is usually the center of a patch that clears first
Feet with ringworm infection – athlete’s foot (Tinea pedis)
Athlete’s foot is caused by a fungus and is medically called tinea pedis. Symptoms may include redness, cracking, itching, and scaling. Some cases may result in blisters on the skin. Athlete’s foot fungus may grow anywhere on the foot, but is most commonly found between the toes.

The fungi that cause athlete’s foot include Trichophyton, Epidermophyton, and Microsporum. Most commonly, the condition is acquired by coming into contact with infected skin, or by coming into contact with fungus in the environment. Swimming pools and locker rooms are common places where the fungi can live.
The most common symptoms of a fungal feet infection are:
- It usually begins between the toes and spreads to the bottom of the foot, sides, or both
- It is possible to spread the infection to your hands by touching an infected foot
- In between your toes and on your soles, there is itching, burning, and stinging
- Red and scaly patches of skin, blisters, painful cracks, and bleeding
- The skin peels off
- An unpleasant smell
- Between the toes, the skin becomes soft and mushy
Hand with ringworm infection (Tinea manuum)
Tinea manuum is a fungal infection of the hand, usually a type of dermatophytosis. Both hands may be affected, and the rash may be different on each hand, with palmer creases turning whitish if the infection has been present for some time. The area can be itchy and look slightly raised. It is possible that your nails will be affected as well.

Scaling is present on the palms or backs of one hand, and the palmer creases are more prominent. Trichophyton rubrum is the most common cause. If you touch another part of the body with a fungal infection, such as an athlete’s foot or fungal infection of the groin, or you come into contact with an infected person or animal, or you touch the soil, or contaminated towels, you may contract the infection.
The most common symptoms of a fungal hand infection are:
- Hands with ring-shaped patches
- The palms are covered with dry, cracked skin
- Palms with deep cracks
- Touching your feet may cause an athlete’s foot
- There is a possibility that the infection will spread to the fingernails (see below).
- Often mistaken for dry, thick skin or extremely dry skin
Nails with ringworm infection (Tinea unguium)
Infection of the nails by fungus, onychomycosis is known as tinea unguium. Nails may become discolored, thicken, and separate from the nail bed if they become white or yellow. Fingernails and toenails may be affected, but toenails are more commonly affected. Lower leg cellulitis can be a potential complication. →

Onychomycosis is caused by a variety of fungi, including Dermatophytes and Fusarium. People with athlete’s foot, other nail diseases, peripheral vascular disease, and poor immune function are at risk. About 10 percent of adult populations are affected by onychomycosis, particularly older adults. It is more common in males than in females.
The most common symptoms of a fungal nail infection are:
- Cracked nails
- The infection can spread to more than one nail
- It begins with the thickening of the nail bed (nail bed tissue).
- It commonly develops in people who have athlete’s foot for a long period of time
- If the nails are thickened, they may lift from the nail bed
- Nails disappearing (with time, you’ll see fewer nails)
- Discoloration and thickening of the nails
- Infected toenails are more common than infected fingernails
Groin with ringworm infection – jock itch (Tinea cruris)
Known as jock itch, tinea cruris is a contagious, superficial fungal infection of the groin region that occurs most commonly in men and in warm, humid climates. There is typically a red raised rash over upper inner thighs that is intensely itchy and scaly with a curved border.

Sports clothing or towels contaminated with infected fungi are often found in this area. It is often associated with athletes’ foot or fungal nail infections. Children are unlikely to be affected by it. Symptoms of inverse psoriasis, erythrasma, seborrheic dermatitis, and candidal intertrigo may be similar to those of fungal groin infection. In order to determine what kind of problem you have; it may be necessary to microscopically examine skin scrapings or to culture them.
The most common symptoms of a fungal groin infection are:
- An initial sign: The crease between the leg and the body is red (brown or gray in dark skin) and swollen.
- Itchy and painful skin can be caused by an infection, but it is not always the case
- Skin that is infected often feels scaly and has raised borders
- Rash spreads to the groin, then slowly spreads to the inner thighs, waist, and buttocks
- Cracks, flakiness, and peeling can occur on the skin
Beard area with ringworm infection (Tinea Barbae)
Fungal infections of the hair are called tinea barbae. Tinea barbae is caused by a dermatophytic infection around the bearded area of men. Generally, the infection appears as a follicular inflammation or granulomatous lesion on the skin. This is one of the causes of folliculitis. The disease is more common among agricultural workers, as it is transmitted more frequently from animal to human than human to human.
Trichophyton mentagrophytes and Trichophyton verrucosum are the most common causes. It is possible to contract the infection from infected animal hair on the skin of a human occasionally.
The most common symptoms of a fungal beard area infection are:
- Redness and swelling are intense
- Fatigue and exhaustion can be felt
- Lymph nodes that are swollen
- The appearance of acne, folliculitis, or another skin condition
- Bumpy skin filled with pus
- A loss of hair (hair often grows back after ringworm is treated)
- Open, raw skin
- Fluid-weeping soft, spongy skin
Scalp ringworm (Tinea capitis)
Tinea capitis (also known as “scalp ringworm“, “ringworm of the hair“, “ringworm of the scalp“, “herpes tonsurans“, and “tinea tonsurans“) is a type of dermatophytosis that affects the scalp. Dermatophytes such as Trichophyton and Microsporum infect the hair shaft and cause the disease.

The clinical presentation is usually one or more patches of hair loss, sometimes with a ‘black dot’ pattern (often broken off hairs), itching, scaling, along with inflammation, and pustules. Children, especially boys, are more likely to suffer from tinea capitis than adults.
The most common symptoms of a fungal scalp infection are:
- Itching that is intense
- Scaly bald patches
- The lymph nodes are swollen
- The scalp is covered with thick, crusty patches of baldness
- The sores are open and oozing pus
- Bald spots with black dots
- The area is raised, spongy, and inflamed
Who gets ringworm?
Everyone can develop ringworm, no matter where they live. The following factors increase your risk of getting ringworm:
- Living in a tropical environment
- Excessive sweating
- When sharing razors, towels, clothes, and other items
- Heat and humidity
- Do not wash and dry your feet well before putting on shoes and socks in a locker room or pool
- Living in close proximity to others, such as in military housing
- Play contact sports, such as wrestling, football, or rugby
- Having diabetes
- Overweight or obese
- Wear clothes that chafe your skin
Sources
https://www.aad.org/public/diseases/a-z/ringworm-causes
https://www.mayoclinic.org/diseases-conditions/ringworm-body/symptoms-causes/syc-20353780
https://www.healthline.com/health/ringworm
https://www.cdc.gov/fungal/diseases/ringworm/index.html
https://www.webmd.com/skin-problems-and-treatments/what-you-should-know-about-ringworm
